Gastroenterology
Patient Information and FAQs
Patient Information & FAQs
Pre-Procedure Advice
Oesophageal manometry and pH studies
Using a sodium citrate Micro-Enema
The RUH has a range of leaflets available about endoscopy tests that can be found on this page.
Post-Procedure Advice
ERCP (Endoscopic retrograde cholangiopancreatography)
Patient Initiated Follow Up (PIFU)
Patient Information
Gastric Antral Vascular Ectasia
Iron deficiency anaemia (IDE), Having Investigations for
Oesophageal dilation, having an
Frequently Asked Questions
- I am struggling to obtain my pancreatic enzyme supplements e.g. Creon, what should I do?
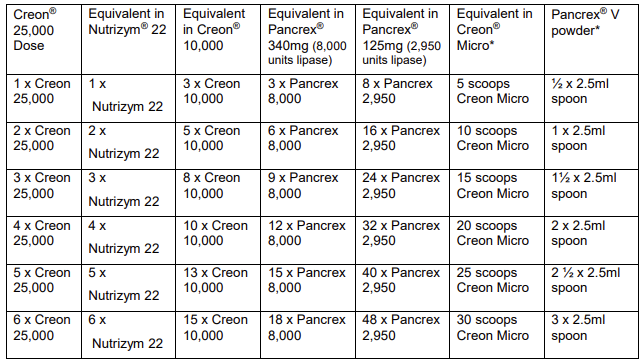
There is an international supply issue surrounding pancreatic enzyme replacement therapy (PERT – under the product brands: Creon®, Nutrizym® and Pancrex®). These intermittent supply issues mean some people are running out of PERT, or experiencing difficulties or delays in accessing PERT.
You can read the international advice for patients available here.
Below is the conversion of your dose to another brand should you need it.
- I have received a letter stating I no longer need colon polyp surveillance. Where can I find out more?
Please take a look at the Colon Polyp Advice provided by the British Society of Gastroenterology.
- I am concerned about bowel cancer, where can I learn more about the available screening?
Please take a look at the information on Bowel cancer screening provided by
'Patient UK', the national NHS information site
- I am concerned I may have an increased risk of bowel cancer due to my family history.
Some people have an increased risk of colorectal cancer if they have close relatives who have developed colorectal cancer. This risk is given as detailed below as it varies between families. The recommendations for further investigations in the different groups may vary throughout the country. You should talk with your doctor if you have members of your family who have had colorectal cancer; sometimes they may refer you to the local genetics service that will send you a family history questionnaire and if necessary discuss your family history with you.
High risk
High risk people are those with certain inherited conditions, which include familial adenomatous polyposis (FAP), hereditary non-polyposis colorectal cancer (HNPCC), and some other syndromes including Peutz-Jegher's syndrome and juvenile polyposis syndrome. These conditions are very rare; three or more affected relatives in a first-degree kinship with each other less than fifty years old would be a risk factor these conditions. Relatives of patients with FAP are offered investigations every year from age 13-15 years until age 30, and 3-5 yearly thereafter until age 60. Relatives of patients with HNPCC are usually advised to have regular bowel screening from the age of 25, or five years earlier than the age their youngest affected relative developed colorectal cancer.
High-moderate risk
People who have a three or more first-degree relatives over 50 years old (mother, father, brother, sister, child) who have had colorectal cancer, or two affected relatives less than 60 years old in a first-degree kinship with each other, or two affected relatives with a mean age less than 60 years old in a first-degree kinship will be offered five yearly colonoscopy from age 50 until 75 years.Moderate risk
People with only one first-degree relative affected by colorectal cancer aged under 50 years or with only two first degree relatives who have had colorectal cancer over 60 have a moderate risk of developing colorectal cancer. These people should be offered a single colonoscopy at age 55 years. If the investigation is normal, then no further investigations (other than the normal bowel cancer screening programme) are recommended.
Low risk
People with family histories that are different to those listed above are classified as low risk, as their risk is similar to the population in general. These people do not need any further investigations (other than the normal bowel cancer screening programme).

