Upper GI
Pancreatic Cancer
Pancreatic Cancer
|
On this page: Overview Causes Symptoms Diagnosis & Assessment Treatment Options Prognosis Related Links & Information |
Overview of Pancreatic Cancer
The pancreas is a large gland which produces digestive juices and insulin. The digestive juices flow down a tube within the pancreas (called the pancreatic duct) and join the intestine at the duodenum. The duodenum is the first part of the small bowel connected to the stomach. The bile duct comes down from the gallbladder and liver and also joins into the duodenum at the same point as the pancreatic duct. The pancreas lies high up in the abdomen. It lies across the body behind the stomach. It is at about the level where the ribs join the bottom of the breast bone.
Pancreatic cancer is relatively uncommon. It affects in 1 in 10,000 people each year in the United Kingdom. There are several different types of pancreatic cancer but the vast majority (9 out of 10) develop from the cells that line the pancreatic duct. These cancers are described as "adenocarcinomas".
As cancer cells grow within the pancreatic ducts, they enlarge and can either block the main pancreatic duct or bile duct which lies next to it. This can stop the drainage of pancreatic fluid or bile into the duodenum.
As the cancer grows larger it can invade the tissues around the pancreas – such as the duodenum, stomach or liver. Cancer cells can also break away and spread through lymph channels to lymph nodes or to other parts of the body – such as the liver, lungs or bones (these are known as metastases or secondaries).
Causes
The exact trigger which causes a cell to become abnormal and develop into a cancer is unclear. Many people develop cancer of the pancreas for no obvious apparent reason. However, certain risk factors do increase the chance that pancreatic cancer might develop. These include:
- Ageing
It is more common in older people. Most cases are in people over the age of 65 - Genetic factors
Some families have a higher incidence of pancreatic cancer than average - Diet
Eating a fatty diet seems to increase the risk. Eating fruit and green vegetables seems to be protective - Smoking
This habit increases the risk of pancreatic cancer as well as many other types of cancer
Chronic pancreatitis
This is a form of persistent inflammation of the pancreas. Most cases are caused by excess alcohol consumption.
Symptoms
Symptoms of a blocked bile duct
In most cases pancreatic tumours develop in the pancreatic duct close to the point where the bile duct enters the duodenum. A small tumour may not cause any symptoms at first. However, as the tumour grows it can cause a blockage of the bile duct and prevent the flow of bile from the liver into the duodenum which leads to:
- Jaundice
Yellowing of the skin and eyes caused by bile building up within the liver and seeping into the blood stream - Dark urine
Caused by jaundiced blood being filtered by the kidneys - Pale faeces
As bile cannot get into the gut, the absence of bile means that faeces lose their normal brown colour and become very pale - Itching
Caused by a build-up of bile within the blood stream - Pain
Is often not a feature at first
Other symptoms
As the cancer continues to grow then further symptoms might develop. These include:
- Pain in the upper abdomen. This is usually in the middle of the back
- Feeling generally unwell and losing weight
Symptoms when the bile duct is not blocked
Symptoms that might develop with the pancreatic duct – when the bile duct is not blocked
In these cases food is not well digested because of the absence of pancreatic fluid. This can cause the motions to be smelly and pale, and produce weight loss.
Diagnosis & Assessment
Initial assessment
There are many causes for jaundice and the other symptoms listed above (e.g. gallstones, hepatitis, drug reactions). Therefore, if you develop jaundice or any of the other symptoms described, then some initial tests are arranged.
Usually, these include an ultrasound scan of the abdomen – intended to look at the bile ducts, liver, gallbladder and pancreas, as well as various blood tests. These initial tests can usually give a good idea of the cause of jaundice and whether it is due to a blockage within the pancreas.
MRCP (Magnetic resonance cholangiopancreatography)
This is a type of magnetic resonance imaging. An MRI scan uses a strong magnetic field and radio-waves to create pictures on a computer of tissues, organs and other structures inside your body. You can’t have an MRI if you have any metal inside your body (e.g. hip or knee replacements or a pacemaker).
An MRI can be used to image the bile ducts, and show whether a cancer is blocking the flow of bile. It can also show whether the cancer has grown into any other structures around the pancreas as well as provide information about whether it has spread to other parts of the body.
CT scan
This is commonly used to assess pancreatic cancer. Again, this can help image the structures around the pancreas to help understand whether it has spread or not.
Endoscopic ultrasound (EUS)
This uses an endoscope, a thin flexible telescope which is passed through the mouth into the oesophagus, stomach and small bowel next to the pancreas. The endoscope contains fibre-optic channels which allow light to shine down through the scope to visualize the lining of the stomach.
An endoscopic ultrasound is fitted with a tiny ultrasound scanner at the tip, which can obtain pictures of structures next to the stomach and duodenum – such as the pancreas.
Laparoscopy
This procedure involves looking inside the abdominal cavity using a laparoscope. This is thin telescope with a light source which can be used to directly visualize the abdominal contents. The laparoscope is passed into the abdomen through a small incision in the skin under general anaesthetic.
More about Laparoscopic Procedures
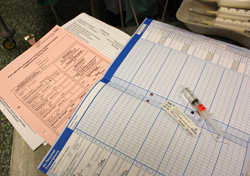
ERCP (endoscopic retrograde cholangiopancreatography)
ERCP uses another form of endoscopy to allow direct visualization of the lining of the stomach and duodenum. Using this technique, the opening of the pancreatic and bile ducts into the intestine can be examined and dye injected from the endoscope into the bile and pancreatic ducts. This is done via a plastic tube inserted through the endoscope.
X-ray pictures can then be taken of the pancreatic ducts which can provide an outline of a tumour or look for other causes of narrowing within these ducts.
Additionally, some treatments can be performed using this type of endoscope. For example, a stent can be placed across a narrowed part of the duct to relieve any blockage.
Assessing the extent and spread
If pancreatic cancer is confirmed or strongly suspected from these initial tests, then they will be analysed to provide information about the “stage” of the cancer. The aim of this staging process is to find out:
- How much the tumour within the pancreas has grown, and whether it has grown into any of the structures around the pancreas
- Whether the cancer has spread to involve local lymph nodes
- Whether the cancer has spread to other parts of the body (metastasized)
Often combinations of tests are needed to find out the stage of the cancer. This information helps us to advise on the best treatment options and also gives a reasonable indication of the outlook (prognosis).
Biopsy
A biopsy of a suspected tumour can confirm the diagnosis. A biopsy is a very small sample of tissue that is removed from a part of the body. This sample is then examined under the microscope to look for cancer cells.
In pancreatic cancer a biopsy can be taken during an ERCP. Sometimes, a biopsy is taken by using a long, fine needle which is passed through the wall of the abdomen and guided to a suspected tumour by using ultrasound or CT scan.
However, if surgery is being considered to remove a suspected pancreatic tumour, then a biopsy is not always done. This is because there is a risk that taking a biopsy can cause some cancer cells to spread.
Treatment Options
Treatment options which may be considered include surgery, chemotherapy and radiotherapy. The choice of treatment in each case depends on various factors such as the stage of the cancer (how large the cancer is and whether it has spread) and your general health.
All the available options will be discussed in detail with a specialist, who will know your case in detail. In this discussion it will be possible to give a description of the pros and cons of different treatments, likely success rates, possible side effects, and other details about various treatment options.
The discussion with your specialist will include an overview of the potential aims of treatment. For example:
- Treatment may aim to try and cure the cancer. Some pancreatic cancer can be cured if they are treated in the early stages of the disease. If the cancer remains localised to the pancreas and has not spread, then such treatment is possible.
- Treatment may aim to control the cancer. If a cure is not possible, either because the cancer has spread too far or because someone’s general health is not good enough to tolerate potentially curative treatment, then treatment may be used to try and limit the growth or spread of the cancer so that it progressed less rapidly.
- Treatment may aim to ease symptoms. If a cure is not possible or if treatments used to try and reduce the size of the cancer are also difficult to tolerate, then treatment may be aimed at easing the symptoms of the cancer. This might include the use of pain killers, nutritional supplements to help with feeding, or other techniques to help keep free of pain or other symptoms.
Surgery
If the cancer is at an early stage, then there is a chance that surgery can be curative.
Such surgery is quite complex and involves removing a significant part of the pancreas, as well as some of the surrounding structures such as the duodenum, stomach and bile ducts. The surgery is long and involved and can have significant risks.
Surgery is only considered if the cancer is small and localised to the pancreas and patients are fit enough to tolerate such major surgery.
If the cancer is at a later stage, then surgery is not an option to cure the disease. However, some surgical techniques can still be used to try and improve symptoms. These might include a bypass procedure to alleviate blockage caused by the cancer. Other techniques might involve using a stent that is inserted into the bile duct. These stents are small, rigid tubes made of plastic or metal which help to keep a bile duct or channel open. Usually such stents are inserted using an endoscope.
Chemotherapy
Chemotherapy uses anti-cancer drugs to kill cancer cells or stop them from growing. The aim of this treatment is to kill as many cancer cells as possible and try and reduce the size of the cancer and slow its growth.
Radiotherapy
Radiotherapy uses high energy beams of radiation which are focused on cancer tissue. This energy kills cancer cells or stops them from growing. Radiotherapy can be used alone or in combination with other treatments such as chemotherapy.
Prognosis / Outlook
If pancreatic cancer is diagnosed and treated at an early stage then there is a chance of cure with surgery. Generally, the smaller the tumour and the earlier it is diagnosed, the better the prognosis.
However, many pancreatic cancers are advanced before they cause symptoms and are diagnosed. A cure in such a situation is unlikely. However, treatments may slow down the progression of the cancer.
Our specialists work as part of the wider Avon, Somerset and Wiltshire Cancer Network. In each case, our patients are discussed by a large number of specialists within a Multi-Disciplinary Team. This includes specialists both at the Royal United Hospital and at the Cancer Centre at the Bristol Royal Infirmary (UBUHT) All potential treatment options are discussed in detail with our Team and patients.

